Or try one of the following: 詹姆斯.com, adult swim, Afterdawn, Ajaxian, Andy Budd, Ask a Ninja, AtomEnabled.org, BBC News, BBC Arabic, BBC China, BBC Russia, Brent Simmons, Channel Frederator, CNN, Digg, Diggnation, Flickr, Google News, Google Video, Harvard Law, Hebrew Language, InfoWorld, iTunes, Japanese Language, Korean Language, mir.aculo.us, Movie Trailers, Newspond, Nick Bradbury, OK/Cancel, OS News, Phil Ringnalda, Photoshop Videocast, reddit, Romanian Language, Russian Language, Ryan Parman, Traditional Chinese Language, Technorati, Tim Bray, TUAW, TVgasm, UNEASYsilence, Web 2.0 Show, Windows Vista Blog, XKCD, Yahoo! News, You Tube, Zeldman
Dr. Sebastian Podlipnik
English-speaking dermatologist in BarcelonaPhotodynamic therapy in dermatology and skin cancer prevention
Photodynamic therapy is an excellent treatment that we have been using for many years in dermatology. It is useful for the prevention of skin cancer in people with photodamage and actinic keratosis (cancerization field) and also to improve photoaging.
My name is Sebastian Podlipnik and I am a dermatologist at the skin cancer unit of the Hospital Clínic de Barcelona. During my years of experience, I have treated hundreds of patients with skin cancer and I continue to promote preventive behaviors to reduce its incidence. That is why minimally invasive treatments such as photodynamic therapy can help us to improve the quality of life of my patients.
What is photodynamic therapy?
Photodynamic therapy is a non-invasive treatment that requires a photosensitizing cream (a chemical compound that is activated by light) to be used on the area to be treated and a source of red or blue light that will activate this photosensitizing compound and will destroy only the abnormal (pre-cancerous) cells, but without affecting the surrounding healthy tissue. In other words, it is a very specific treatment to eliminate the abnormal cells in the photoexposed areas.
It is approved and used mainly in dermatology to treat:
- Actinic keratosis (precancerous) (Luo et al., 2024)
- Superficial basal cell carcinoma and nodular carcinoma (Collier et al., 2020)
- Squamous carcinoma in situ (Bowen's disease)
- Photoaging and skin rejuvenation (Tierney et al., 2009)

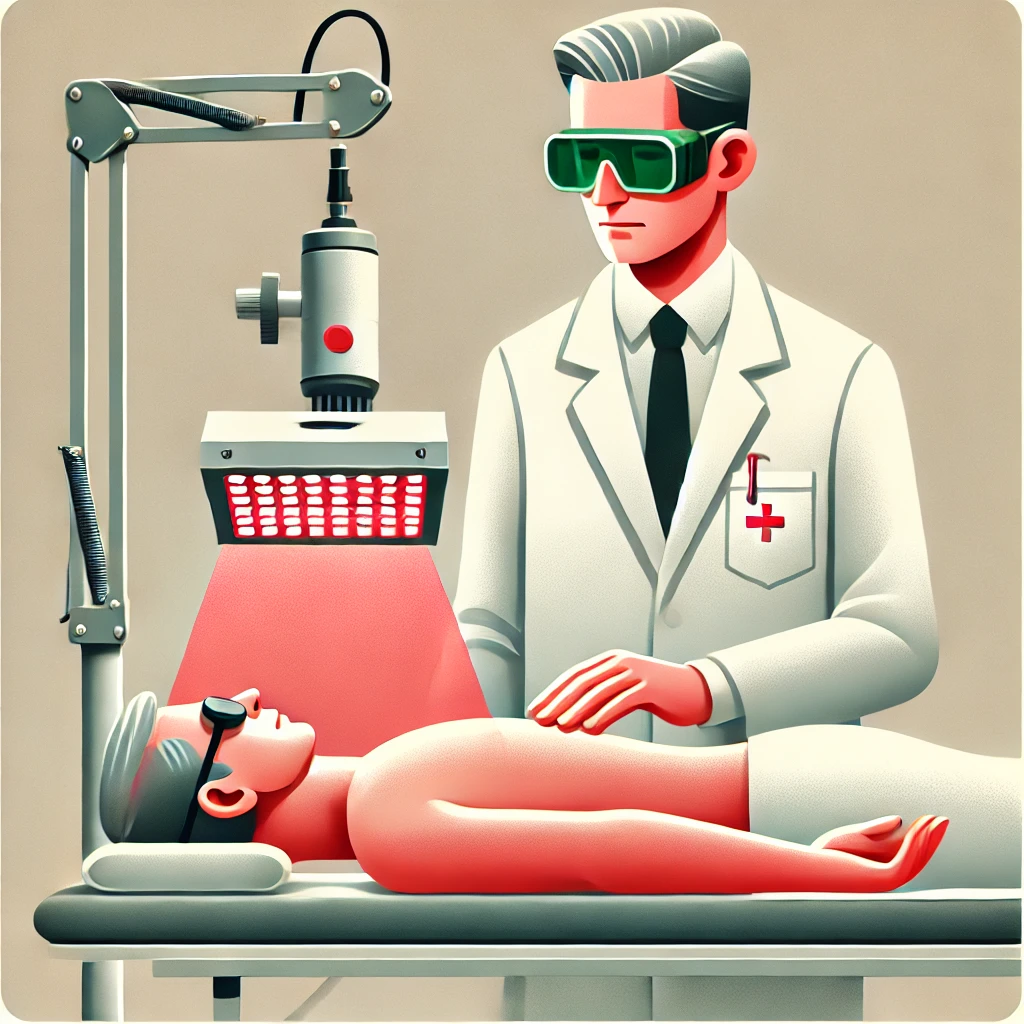
Patient who has been directly exposed to the sun all his life due to his work. Since a few years ago he notices the appearance of many "scratchy red spots" on the scalp and forehead. In this case they correspond to multiple actinic keratoses that may predispose this patient to develop skin cancer.
How effective is photodynamic therapy?
Photodynamic therapy is a highly effective treatment for precancerous lesions such as actinic keratosis with elimination rates of 70% to 90% after a single session, according to different studies. It has also been shown to be effective in the treatment of superficial basal cell carcinoma and in skin rejuvenation, as it improves skin quality by stimulating collagen production. Combination with technologies such as fractional CO2 laser can further enhance its efficacy by improving the penetration of the photosensitizer.
How is photodynamic therapy applied?
Although there are several modalities to perform photodynamic therapy I will explain step by step the conventional way. Later I will also briefly discuss a second modality that we apply today called "daylight photodynamic therapy".
1- Preparation of the area to be treated
Depending on each case we will prepare the area a few days before applying photodynamic therapy. In the case of patients with cancerization field and many hypertrophic actinic keratoses (very crusty or scabby), we will recommend using a keratolytic cream to clean the affected area a little. In this way we will achieve that the photosensitizer has better penetration into the skin and can reach the layers of the epidermis that we need to treat.Quote
2- Application of the cream with or without CO2 laser
Already in the day of the consultation, the patient will be scheduled for the application of the photosensitizing cream. (Methyl aminolevulinate [MAL, Metvix®] or 5-aminolevulinate [ALA, Ameluz®] available in Spain).
Depending on each case, we can simply apply the cream or also apply a fractionated CO2 laser that will allow us to make channels in the skin, a concept known as drug delivery. This is the method I use the most in my practice in Barcelona, Spain.
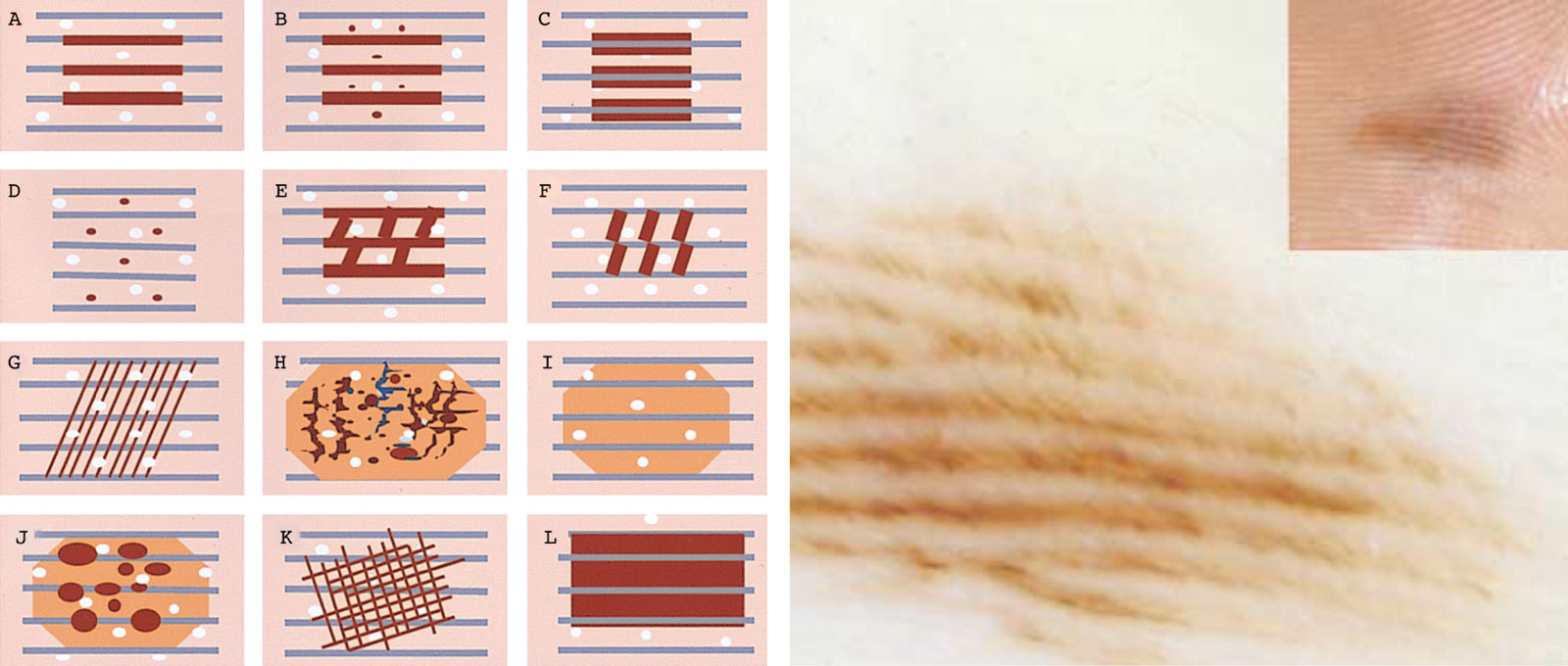
Drug delivery means that we use fractionated CO2 laser that creates microchannels in the epidermis, allowing the photosensitizer to penetrate deeper and more evenly into the skin. This technique improves treatment efficacy and can reduce drug incubation time. The following figure best exemplifies this concept.

Illustration showing the concept of drug delivery in the skin. With the CO2 laser, small channels are created in the epidermis through which the photosensitizer can enter in photodynamic therapy.
If we only apply the cream without the laser, absorption will be more superficial, which may be sufficient in thinner lesions or sensitive areas. In contrast, by combining PDT with fractional CO2 laser, we achieve more effective penetration, especially in thicker lesions or in patients with extensive skin damage.
3- Incubation
Depending on the photosensitizer chosen (MAL or ALA) and whether we perform CO2 lasers beforehand to create microchannels in the skin. it will take 1-3 hours for the drug to reach the affected skin cells. and the photosensitizer binds to these cells. During this time, the patient should avoid direct exposure to light to prevent premature activation of the drug.
4- Application of LED light (photons)
After this wait, we will finally apply a source of light energy (high energy red light) that will deliver the necessary photons to activate the photosensitizing molecules and selectively destroy the pre-cancerous or sun-damaged cells.
When red light strikes the treated skin, the previously absorbed photosensitizer generates reactive oxygen species (ROS), which causes selective destruction of the affected cells without damaging healthy tissue. Red light (generally 630-635 nm) is ideal for photosensitizer activation, as it efficiently penetrates the skin without generating excessive thermal damage.
What other photodynamic therapy modalities are available?
I have already told you about two forms of photodynamic therapy, conventional and photodynamic therapy combined with CO2 laser. There is also a third form of photodynamic therapy known as "daylight"..
What is daylight photodynamic therapy?
Photodynamic therapy with natural light or daylight is a fairly simple modality that takes advantage of sunlight (instead of the red LED lamp) to activate the photosensitizing medication applied to the skin.
Unlike conventional lamp therapy, this modality is less painful, as drug activation occurs gradually with sun exposure over approximately 2 hours. Quote
What are the disadvantages of daylight photodynamic therapy?
The main disadvantages of daylight photodynamic therapy are that its efficacy depends on the intensity of sunlight, so it is not recommended on cloudy days or in winter, and that it can cause redness and flaking of the treated skin in the days following the procedure. Also, in some cases, the response to treatment may be slower compared to conventional lamp therapy.
Is photodynamic therapy painful and what effects will be seen in the following days?
Photodynamic therapy (PDT) can generate a burning or stinging sensation during the application of light, especially in the conventional modality with LED lamp, since the activation of the photosensitizer occurs intensely and rapidly. On the other hand, in PDT with natural light, drug activation is progressive, so the treatment is less painful.
After the session, it is normal for the skin to show redness, slight swelling and peeling in the following days, similar to a mild sunburn. In some cases, small scabs may appear on the treated areas, which is part of the skin regeneration process. These effects usually disappear in one or two weeks, leaving a renewed skin with better texture.
Frequently asked questions from patients
How many sessions do I need?
In most cases, one session is sufficient. However, an annual treatment is necessary to maintain the results.
¿Puedo hacer vida normal después del tratamiento?
Yes, but avoid sun exposure for 48 hours. There may be redness and mild peeling, but you can continue with your daily activities using sunscreen.
Is photodynamic therapy painful?
The LED lamp modality may cause burning or stinging, although we will use techniques to minimize this. The Daylight-PDT technique is less painful due to its gradual activation.
What care should I follow afterwards?
Apply moisturizer and sunscreen SPF 50+, avoid the sun and do not scratch the peeling skin. Recovery usually takes 7 to 10 days.
La entrada Terapia fotodinámica en dermatología y prevención del cáncer de piel se publicó primero en Dr. Sebastian Podlipnik.
Cutaneous Horn: What It Is, Why It Forms, and How to Treat It
Cutaneous horn is one of those dermatological curiosities that often surprises people, especially those who have never heard of it. If you’re reading this, you’ve probably been diagnosed with this condition, know someone who has it, or simply found the topic interesting. Whatever the case may be, welcome. Here, I will explain what a cutaneous horn is, why it appears, and how it can be properly treated.
My name is Sebastian Podlipnik, I am a dermatologist at the Hospital Clínic of Barcelona, and I have spent years researching and treating various skin diseases, including those related to sun exposure and skin cancer. I have seen numerous cases of cutaneous horns, and my priority is always to ensure that patients understand what this condition is, why it occurs, and how to treat it effectively.
In this article, I will share my experience with you in a clear way so that you can better understand what it is and what steps to take if you ever encounter this lesion.
What will I talk about in this article?
What is a Cutaneous Horn?
A cutaneous horn is a skin lesion that appears as a rigid protrusion or growth primarily made of keratin, the same protein that makes up our nails and hair. Visually, it can resemble a horn emerging from the skin, which is where its name comes from. Although its appearance may alarm some, the cutaneous horn is not a disease in itself, but rather a manifestation of an underlying skin problem.
These lesions vary in size, with some being small while others can reach several centimeters in length. A cutaneous horn can appear anywhere on the body, although it is more common in sun-exposed areas such as the face, scalp, ears, and hands. It affects both men and women, although it is more common in people over 60 years of age. (Copcu et al., 2004).

Why Does a Cutaneous Horn Form?
A cutaneous horn forms due to an accumulation of keratin in the skin, but this buildup is not random. It is related to an underlying skin lesion. This is crucial from a dermatological perspective, because although the horn itself may not be dangerous, it signals that benign, precancerous, or even malignant conditions could exist at the base of the cutaneous horn. (Bondeson, 2015).
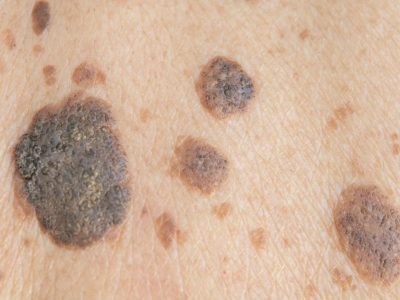
Is a Cutaneous Horn Dangerous?
One of the most common questions I hear in consultations is whether a cutaneous horn is dangerous. The short answer is: it depends. Not all cutaneous horns are dangerous, but some can be secondary to a malignant lesion. What really matters is the base of the lesion, as I mentioned earlier. Many cutaneous horns develop over benign lesions, such as seborrheic keratosis, which are not dangerous. However, in other cases, the cutaneous horn may form over an actinic keratosis (a precancerous lesion), or, in more serious cases, over a squamous cell carcinoma, a type of skin cancer. (Reddy et al., 2013).
Cutaneous Horn and Skin Cancer
Cutaneous horns are most commonly associated with malignant lesions in people over the age of 50, especially those with prolonged sun exposure. In fact, recent studies suggest that around 20% of cutaneous horns are related to skin cancers, particularly squamous cell carcinoma. Therefore, although it is not always dangerous, it is essential that any cutaneous horn be evaluated by a dermatologist to rule out serious issues. (Yu et al., 2019).

How is a Cutaneous Horn Diagnosed?
The diagnosis of a cutaneous horn is usually straightforward due to its characteristic appearance. However, it is crucial to perform a biopsy in most cases to evaluate the underlying lesion. Through the biopsy, we can determine whether the base of the lesion is benign, precancerous, or malignant, which allows us to decide on the most appropriate treatment. (Meyerson et al., 2017).
When is a Biopsy Necessary?
I recommend a biopsy in most cases of cutaneous horn, especially if the patient has a history of prolonged sun exposure or skin cancer. The biopsy not only provides an accurate diagnosis but also gives us peace of mind by determining if there is an underlying risk that needs to be addressed. (Morgan et al., 2020). In some cases, a dermatoscopic examination of the lesion can help us make an accurate diagnosis and avoid a biopsy.

Treatment in Cases of Malignancy
When the biopsy reveals a malignant lesion, the treatment can be more complex. In some cases, a more extensive surgery (widening the margins) is necessary to ensure that all affected tissue is removed. This is particularly important in cases of squamous cell carcinoma. (Mounsey et al., 2018).
Treatment Options:
- Surgical Excision: The horn is removed along with the underlying lesion, and this is the method of choice in most cases.
- Cryotherapy: The lesion is frozen with liquid nitrogen to remove it. This is especially indicated if the cutaneous horn is related to benign lesions or actinic keratosis.
- Curettage and Electrodessication: It involves scraping the lesion and destroying the base with electric current. Like cryotherapy, it is reserved for cases of benign lesions or actinic keratosis.
- Photodynamic Therapy: It uses light and a photosensitizer to destroy precancerous cells and is used for premalignant lesions or squamous cell carcinoma in situ (located in the most superficial layer of the skin – the epidermis). (Simmons et al., 2017).
Prevention of Cutaneous Horn
Preventing the appearance of these lesions is closely related to sun protection. Most of the lesions that can produce a cutaneous horn are linked to accumulated sun damage, so protecting the skin is key to reducing the risk of developing cutaneous horns. (D’Orazio et al., 2016).
Prevention Tips:
- Apply sunscreen daily, even on cloudy days.
- Avoid sun exposure during peak hours.
- Wear protective clothing and wide-brimmed hats.
- Have regular dermatological check-ups, especially if you have a history of prolonged sun exposure.
Frequently Asked Questions About Cutaneous Horn
Is a Cutaneous Horn Always Malignant?
No, many cutaneous horns are benign, but they should always be evaluated by a dermatologist to rule out more serious issues.
How can I tell if I have a cutaneous horn?
A cutaneous horn appears as a hard protrusion on the skin, which can vary in size. If you have a lesion that looks like a horn, it is important to have it evaluated by a dermatologist.
Can a Cutaneous Horn Recur After Being Removed?
In some cases, if the underlying lesion is not completely removed, the cutaneous horn can reappear. That’s why it’s crucial to treat both the horn and the underlying tissue.
My Experience with Patients with Cutaneous Horn
Throughout my career as a dermatologist, I have treated many cases of skin cancer and cutaneous horns. What I have learned is that early detection and treatment are key to preventing major complications. I advise my patients to pay attention to any changes in their skin, especially in sun-exposed areas, and to consult a dermatologist if they have any concerns.
Conclusion
A cutaneous horn may seem like a simple curiosity, but its evaluation and treatment are essential to avoid complications. Whether benign or malignant, it should be assessed by a dermatologist to ensure proper treatment. Remember that prevention, especially through sun protection, is your best tool to avoid this type of lesion.
If you have more questions about cutaneous horns or other dermatological conditions, feel free to leave your comment below, and if you have one, don’t hesitate to request a consultation. I’m here to help you take care of your skin.
La entrada Cuerno Cutáneo: Qué es, por qué se forma y cómo tratarlo se publicó primero en Dr. Sebastian Podlipnik.
Oral Sunscreen: Is It the Best Option to Protect Your Skin from Sun Damage?
When we think about caring for our skin, we usually consider sunscreen lotion as the first line of defense against sun damage. However, in recent years, a new strategy has been gaining attention: oral sunscreen.
In this article, I’d like to delve into this complementary approach and explain how it can help you keep your skin better protected from sun damage. If you’re concerned about premature aging, sun spots, or even skin cancer, keep reading to discover how oral sunscreen can help in your skincare routine.

What will I talk about in this article?
What is Oral Sunscreen and How Does It Work?
Oral sunscreen involves the use of supplements containing active ingredients that protect the skin from the inside against the harmful effects of solar radiation, especially ultraviolet (UV) radiation, but also visible light and infrared. These supplements include antioxidants, vitamins, and carotenoids, which act directly on our cells to reduce damage caused by sun exposure.
The mechanism of action of these compounds is quite interesting. They work primarily as antioxidants and anti-inflammatories. For example, they reduce the formation of reactive oxygen species (ROS), which are the molecules responsible for cellular damage and skin aging. Additionally, some of these ingredients help repair the DNA of cells and strengthen the skin’s immune response against sun damage. (Parrado et al., 2018).
Should We Call It Oral Sunscreen?
The term “oral sunscreen” may not be the most accurate in this context. When we think of sun protection, we usually picture the classic sunscreen that physically or chemically blocks UV rays. Oral supplements, on the other hand, do not directly block UV radiation. Instead, they protect the skin from within, helping to minimize cellular damage that has already occurred.
For this reason, I prefer to see oral sunscreen as a way to help the skin cope with sun damage rather than as a preventive barrier. The most common ingredients in these supplements, such as Polypodium leucotomos or nicotinamide, do not prevent exposure to UV rays. What they do is reduce inflammation, improve DNA repair, and decrease oxidative stress, all key factors in mitigating the cumulative damage caused by sun exposure.
Main Ingredients Used in Oral Sunscreen
- Polypodium leucotomos: This fern extract is probably one of the most studied and recognized for its antioxidant and anti-inflammatory properties. Additionally, it has been shown to help repair the DNA of damaged cells and may prevent sun-related skin disorders, such as photodermatosis. (Parrado et al., 2020).
- Nicotinamide (Vitamin B3): This compound has been shown to be highly effective in preventing non-melanoma skin cancers by improving DNA repair and protecting the skin from sun-induced immunosuppression. (Chen et al., 2014).
- Carotenoids: These are pigments found in brightly colored fruits and vegetables, such as beta-carotene and lycopene. Studies have shown that these compounds are effective in reducing skin pigmentation caused by UVA rays. (Baswan et al., 2020).
- Omega-3 Fatty Acids: The fatty acids found in fish oil are well known for their anti-inflammatory properties. In the context of photoprotection, they help reduce oxidative damage and inflammation caused by sun exposure. (Fania et al., 2021).
Consequences of Cumulative Sun Exposure
Sun damage is not something that is immediately noticeable, but it accumulates over time.. Every time your skin is exposed to the sun, especially without protection, cellular damage occurs that, although not immediately visible, can lead to serious problems over the years. This cumulative damage not only accelerates skin aging—wrinkles, loss of elasticity, and sunspots—but also significantly increases the risk of developing skin cancer.
Over time, constant exposure to UV radiation causes a series of mutations in the DNA of skin cells. These alterations can interfere with the normal process of cellular regeneration, facilitating the development of melanomas and other types of cancer, such as basal cell carcinoma or squamous cell carcinoma. For this reason, combining topical sunscreen with the use of oral sunscreen becomes key in reducing these negative effects in the long term. (Krutmann et al., 2020).

Chronic sun damage is clearly visible in the case of two 61-year-old twin sisters, Jeanne and Susan. Although they share the same genetics, their sun exposure habits have made a significant difference in their appearance. Jeanne, who has avoided prolonged sun exposure, has much smoother and less aged skin, while Susan, who has been regularly exposed to the sun in Florida, shows evident signs of premature aging, such as sunspots and deep wrinkles. A study showed that Susan appears more than 10 years older than Jeanne due to accumulated sun damage. This example highlights how ultraviolet (UV) radiation and a lack of sun protection can accelerate skin aging, underscoring the importance of using sunscreen and adopting habits that limit direct sun exposure.
Product Recommendation:
Lumium Capsules
- Nicotinamide 500 mg
- Polypodium Leucotomos 480 mg
- Beta-carotene
- Resveratrol
- Vitamins C, D3, and E
Lumium not only helps reduce inflammation and repair damaged DNA but also strengthens the skin’s immune response to the sun. This supplement is ideal for those looking for additional protection beyond what topical sunscreen offers. Remember, it’s always the combination that will give you the best results.
What Does Science Say About Oral Sunscreen?
There are numerous studies supporting the benefits of oral sunscreen. For example, a study conducted on humans demonstrated that the extract of Polypodium leucotomos is effective in reducing inflammation and skin damage after exposure to UVB radiation. (Kohli et al., 2017). Likewise, supplementation with carotenoids has demonstrated its ability to reduce erythema caused by UV radiation. (Baswan et al., 2020).
Additionally, nicotinamide has shown promising results in reducing the risk of non-melanoma skin cancer by improving DNA repair mechanisms. (Chen et al., 2014)This, along with the antioxidant effects of other ingredients, makes oral sunscreen a powerful tool for preventing long-term sun damage.
Limitations of Oral Sunscreen
It is important to remember that oral sunscreen should not replace traditional sunscreen. Oral supplements are a complementary tool and should not be seen as a standalone solution. Avoiding the sun with physical measures (staying under an umbrella, avoiding direct sun exposure, using hats and sunglasses, etc.) and the topical application of sunscreens remains the most effective way to block UV radiation directly on the skin.
Another limitation is that The effects of oral sunscreen are not immediate. Most studies suggest that consistent intake over several weeks is required to observe benefits for the skin. So, if you decide to incorporate these supplements, keep in mind that it is a long-term commitment.
Conclusion
In summary, oral sunscreen is a strategy that effectively complements traditional sun protection measures. Although it does not replace topical sunscreens, it helps reduce the impact of sun damage on the deeper layers of the skin. As research progresses, it is likely that we will see new combinations of ingredients that further improve results.
If you’re interested in providing more comprehensive protection for your skin, I encourage you to consider incorporating oral sunscreen into your routine, always alongside a good topical sunscreen and proper skincare habits. Remember, the sun is unforgiving, but with the right protection, we can minimize its impact on our skin. And don’t forget to visit a dermatologist if you have any concerns about your skin or signs of photoaging.

Shall We Start your Transformation?
La entrada Protector Solar Oral: ¿Es la Mejor Opción para Cuidar Tu Piel del Daño Solar? se publicó primero en Dr. Sebastian Podlipnik.
Sebaceous Hyperplasia: Causes and Effective Treatments
Sebaceous hyperplasia is a skin condition that often goes unnoticed until it becomes a cosmetic concern. Although generally harmless, its presence can be worrisome, especially when it affects your appearance. As a dermatologist, I have seen how these small yellowish papules on the face can impact my patients’ confidence.
If you've noticed these persistent bumps, you might be dealing with sebaceous hyperplasia. Don’t worry, in this blog, I'll explain what they are, why they occur, and most importantly, how you can effectively treat them to restore the health of your skin.
What will I talk about in this article?
What is Sebaceous Hyperplasia?
Sebaceous hyperplasia occurs when the sebaceous glands, which are responsible for producing the oil (sebum) that keeps your skin hydrated, become enlarged. This enlargement leads to the formation of small, soft bumps that are often yellowish with a central depression, resembling tiny doughnuts on the skin. These bumps most commonly appear on the face, particularly on the forehead, cheeks, and nose. cita

Although these bumps are not harmful, their appearance can be concerning, especially since they can sometimes resemble more serious skin conditions, such as basal cell carcinoma. As a dermatologist, I emphasize the importance of getting a professional diagnosis to ensure that you are dealing with sebaceous hyperplasia and not something more serious.
Sebaceous hyperplasia can easily be mistaken for more serious conditions. A precise diagnosis is essential for successful treatment.
Dr. Sebastian Podlipnik

Contributed by Ronald Rapini, MD From: Sebaceous Hyperplasia
¿Cómo se ven las hiperplasias sebáceas en dermatoscopia?
La dermatoscopia es una técnica utilizada por los dermatólogos para examinar la piel en detalle, usando un dispositivo especial llamado dermatoscopio. Este aparato permite ver la piel con aumento y luz polarizada, revelando estructuras que no son visibles a simple vista.

Una hiperplasia sebácea es una lesión común que aparece como un pequeño bulto en la piel, generalmente en la cara. Ocurre cuando las glándulas sebáceas, que producen el aceite de la piel, se agrandan. Bajo la dermatoscopia, esta condición se ve como un bultito amarillento con una pequeña depresión en el centro, a veces acompañado de pequeños vasos sanguíneos en su superficie.
What Causes Sebaceous Hyperplasia?
The exact causes of sebaceous hyperplasia are not entirely clear, but studies suggest that several factors contribute to its development: Quote
- Aging and Hormonal Changes: As we age, androgen levels decrease, which stimulates the proliferation of sebaceous glands, particularly on the face, typically beginning around the ages of 30-40.
- Androgen Sensitivity: Sebaceous glands respond to androgens, which increase their activity and size, contributing to the development of sebaceous hyperplasia.
- Sun exposure: Prolonged exposure to UV rays can accelerate the development of sebaceous hyperplasia, particularly on the face.
- Immunosuppressive Treatments: Medications such as cyclosporine A, used in transplant patients, can increase the risk of developing sebaceous hyperplasia.
- Genetic Factors and Syndromes: Some forms of sebaceous hyperplasia are associated with genetic predispositions and syndromes such as Muir-Torre syndrome, although they are much less common.
How to Treat Sebaceous Hyperplasia: My Recommendations
Although sebaceous hyperplasia is benign, many of my patients seek treatment to improve their appearance.

My Perspective as a Dermatologist
Throughout my years of practice and experience as a dermatologist, I have concluded that the most effective treatments for addressing this condition undoubtedly include the following approaches:
Preferred Method
- CO2 laser: In my opinion, the best treatment for eliminating sebaceous hyperplasia is CO2 laser therapy. This laser effectively removes the lesions, leaving the skin much more even. The results are exceptional.Quote
- Topical Retinoids: Once sebaceous hyperplasia has been removed, we recommend the use of topical retinol to prevent the appearance of new lesions. nuevas hiperplasias sebáceas. Este tratamiento no solo ayuda a reducir la producción de sebo y en algunos casos la aparición de nuevas lesiones. Si bien, los dermatólogos lo recomiendan ampliamente no existen tantos estudios de que demuestren su eficacia, es por ello que en casos más graves podemos recomendar un tratamiento oral.
- Oral Retinoids: In more severe cases or when there is a tendency for recurrence, we may offer the use of oral retinoids, always under the supervision of a dermatologist.
CO2 laser ablation is the fastest and most effective solution for treating sebaceous hyperplasia, with full recovery in less than a week.
Dr. Sebastian Podlipnik
Other Treatments
- Electrocautery and Curettage: In contexts where CO2 laser is not available, techniques such as electrocautery and curettage are excellent options that allow for the precise removal of sebaceous hyperplasia.
- Trichloroacetic Acid Peel: Another effective option isFocused chemical peels with TCA at 35-50%.Quote
- Cryotherapy It can be effective if done with caution and expertise. It is preferable to use a cotton applicator instead of the conventional spray method, as the latter can leave white spots or even cause scarring. However, in clinical practice, it may not make much sense given the availability of CO2 laser and other much more effective methods.
- Azelaic Acid and Other Alpha Hydroxy Acids: Known for their anti-inflammatory properties, these acids can help reduce the size and appearance of the lesions. However, retinoids are generally more effective.
Will They Reappear?
Sebaceous hyperplasia lesions generally tend to reappear over time, usually after a few years, although this can vary; in some cases, they may return sooner or later. Topical retinoids can help reduce the likelihood of recurrence, although in practice, oral retinoids tend to offer more consistent results.
Ready to Say Goodbye to Sebaceous Hyperplasia?
If you’ve noticed those small bumps on your face and they’re causing you concern, it’s completely understandable that you’d want to take action. Although sebaceous hyperplasia doesn’t pose a health risk, I know from experience that they can impact how you feel about yourself. Fortunately, there are effective treatments that can help improve the appearance of your skin.

Shall We Start your Transformation?
As a dermatologist with extensive experience in this condition, my goal is to offer you the best treatment options, tailored to your needs. Whether you're considering treatment or simply need guidance, I invite you to schedule a consultation. I’m here to help you find the solution that best suits your skin.
La entrada Hiperplasias sebáceas: causas y tratamientos efectivos se publicó primero en Dr. Sebastian Podlipnik.
Dermatofibroma: what you need to know about this benign tumor
In the wide world of cutaneous lesions, the dermatofibroma stands out as a benign skin lesion, which nevertheless can frighten many patients. Although it is not dangerous, its presence and rapid onset can generate doubts and concerns, even if it is thought to be a malignant lesion. This article is designed to clear all your doubts about dermatofibromas, explaining in detail what they are, why they appear and when it is necessary to seek treatment.

What will I talk about in this article?
What is a dermatofibroma?
Dermatofibroma, also known as fibrous histiocytoma, is a benign soft and fibrous tissue tumor that develops in the skin. They usually present as small, firm, small papules, generally less than 1 cm in diameter. These nodules are more common on the extremities, but can appear anywhere on the body.

Causes and Risk Factors
The exact cause of dermatofibroma remains unknown. However, an association with previous skin trauma, such as insect bites, minor wounds or superficial punctures, has been observed. Often, patients report having suffered some type of lesion in the area where the dermatofibroma appears.
Who gets dermatofibromas?
Dermatofibroma can affect people of all ages, but it can also affect people with is more common in individuals between 20 and 50 years of age, and has a higher prevalence in women. Studies have shown that these tumors constitute approximately 3% of all dermatopathology specimens sent to laboratories.
Why do dermatofibromas appear?
The exact cause of dermatofibroma is not known with certainty. However, it is believed to be a reactive response to minor skin trauma, such as insect bites, scratches or superficial punctures.. Although, in many cases, these lesions appear without any apparent triggering event. It is likely that both inflammatory and neoplastic reactive factors play a role in their development.
Symptoms of dermatofibromas
Most dermatofibromas are asymptomatic and are discovered incidentally. However, some may cause pain, tenderness or itching. They usually present as firm nodules that are brown, red or yellow to the touch, and may retract when compressed laterally, a phenomenon known as the "dimple sign".

Diagnosis
The diagnosis of dermatofibroma is generally is performed by clinical examination, patient history and using dermoscopy. In doubtful cases, a biopsy can be performed to confirm the diagnosis. Below is a typical dermatoscopic image of a dermatofibroma.


Treatment
- Surgical excisionComplete removal of the nodule may be necessary if there is suspicion of malignancy or if the patient desires it for cosmetic reasons. It is the treatment of choice in most cases.
- CryotherapyCryotherapy has been described in some cases for the treatment of dermatofibromas, although in my opinion it is not very useful and does not have good results.
Can dermatofibromas be prevented?
Although dermatofibromas cannot be prevented, it is important to educate patients about the benignity of these tumors and that in most cases they will not require further treatment. We always advise patients to watch for any changes in their skin lesions and that consult a dermatologist if you notice anything unusual, as it could be a malignant lesion..
Conclusion
Dermatofibroma is a common benign lesion that can appear anywhere on the body, especially on the extremities. Although generally harmless, it can cause discomfort and cosmetic concerns in some cases. Diagnosis is usually clinical, supported by biopsy if necessary, and treatment is reserved for symptomatic cases or by patient preference. Patient education is critical to ensure proper understanding and management of these lesions.
References
- Myers, D. J., & Fillman, E. P. (2024). Dermatofibroma. StatPearls. Retrieved from https://www.ncbi.nlm.nih.gov/books/NBK470538/.
- Dermatofibromas: A Review of the Literature. SAGE Journals. Retrieved from https://journals-sagepub-com.sire.ub.edu/doi/10.1177/106689690401200406.
La entrada Dermatofibroma: Lo que necesitas saber sobre este tumor benigno se publicó primero en Dr. Sebastian Podlipnik.
Moles on the soles of the feet and palms of the hands
Greetings to all lovers of skin health and skin cancer prevention! I am Dr. Sebastian Podlipnik, a skin cancer specialist working at the Hospital Clínic in Barcelona. In my dermatological career, I have had the opportunity to study and care for a wide variety of cases, and today I want to immerse you in a topic that often goes unnoticed and is the subject of much controversy: moles on the soles of the feet and palms of the hands.
Have you ever wondered why moles on hands and feet deserve special attention?
Although these small skin "companions" may go unnoticed due to their unusual location, their importance and the care they require are just as crucial as those of any other mole on our body. From their appearance to their possible link to skin cancer, we will explore together the mysteries and concerns surrounding these moles, as well as the steps we can take to keep our skin in optimal health.
Keep reading, because I'm going to tell you everything you need to know!

What will I talk about in this article?
Why are moles on the soles of the feet different from those on the palms of the hands?
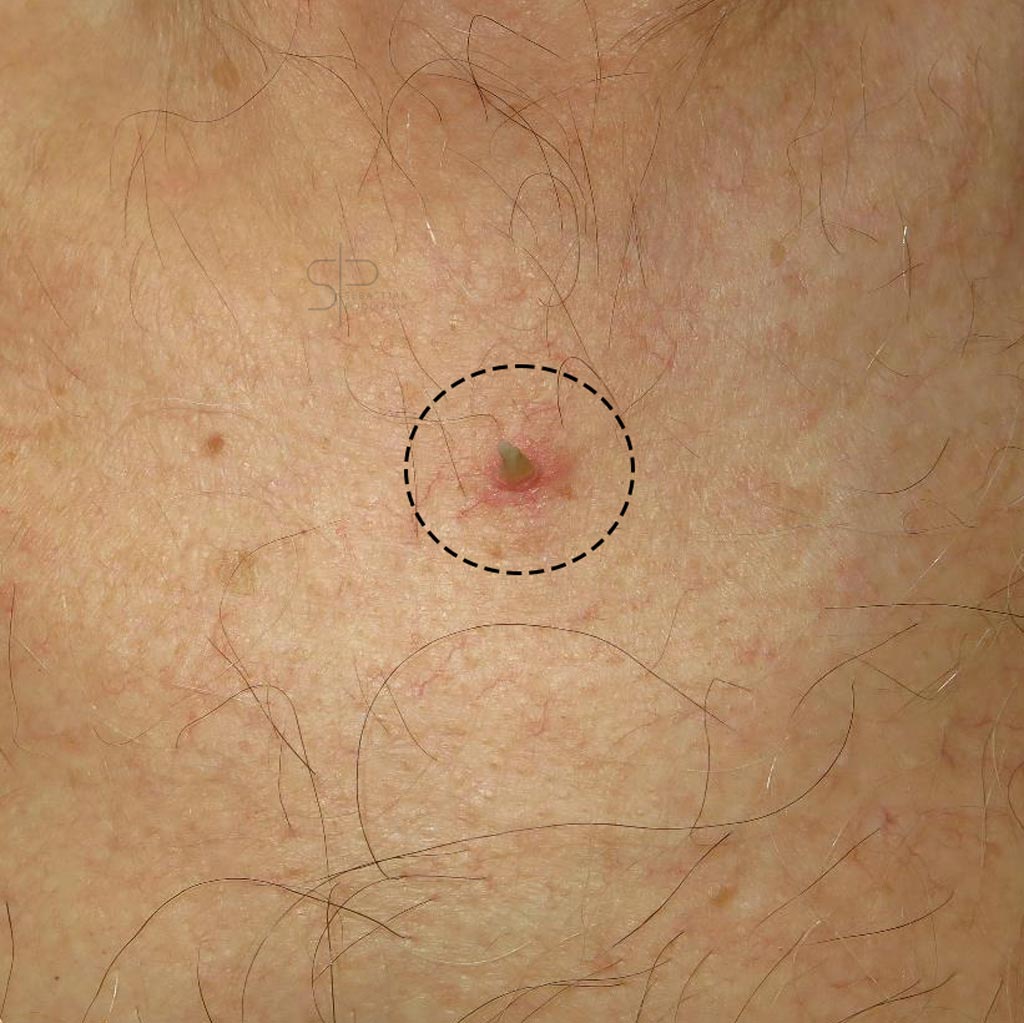
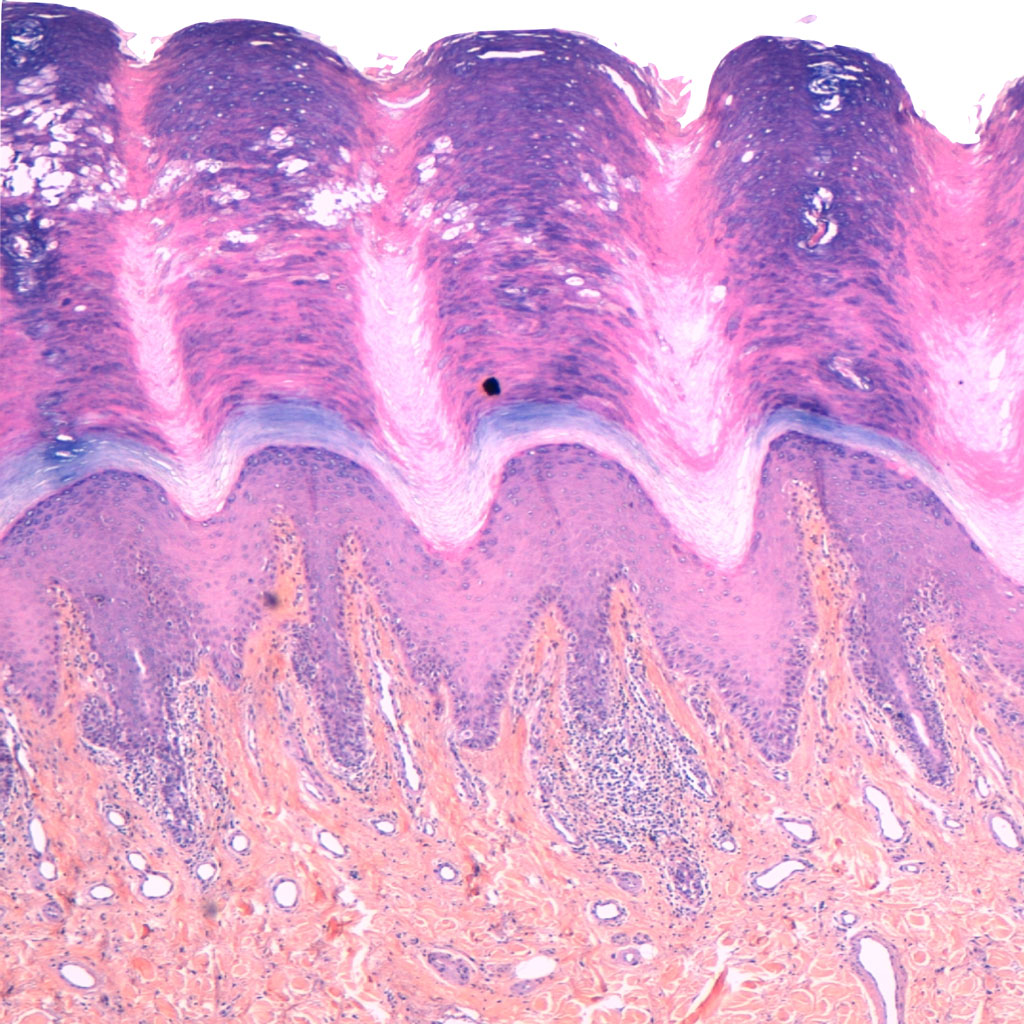
The main reason for moles on the soles of the feet and the palms of the hands is because the skin in this area is different and is called acral skin.. In general terms, the stratum corneum of the epidermis is much thicker and folds giving a fingerprint appearance. This makes moles in these areas acquire different characteristics and in the past it was more difficult to characterize them as benign or malignant.
As you can see in the following images, I have put a magnified photo of these folds and also how they look under the microscope. The skin in this location is very special and that will make the moles on the soles of the skin and the palms of the hands look totally different as well.
Acral skin
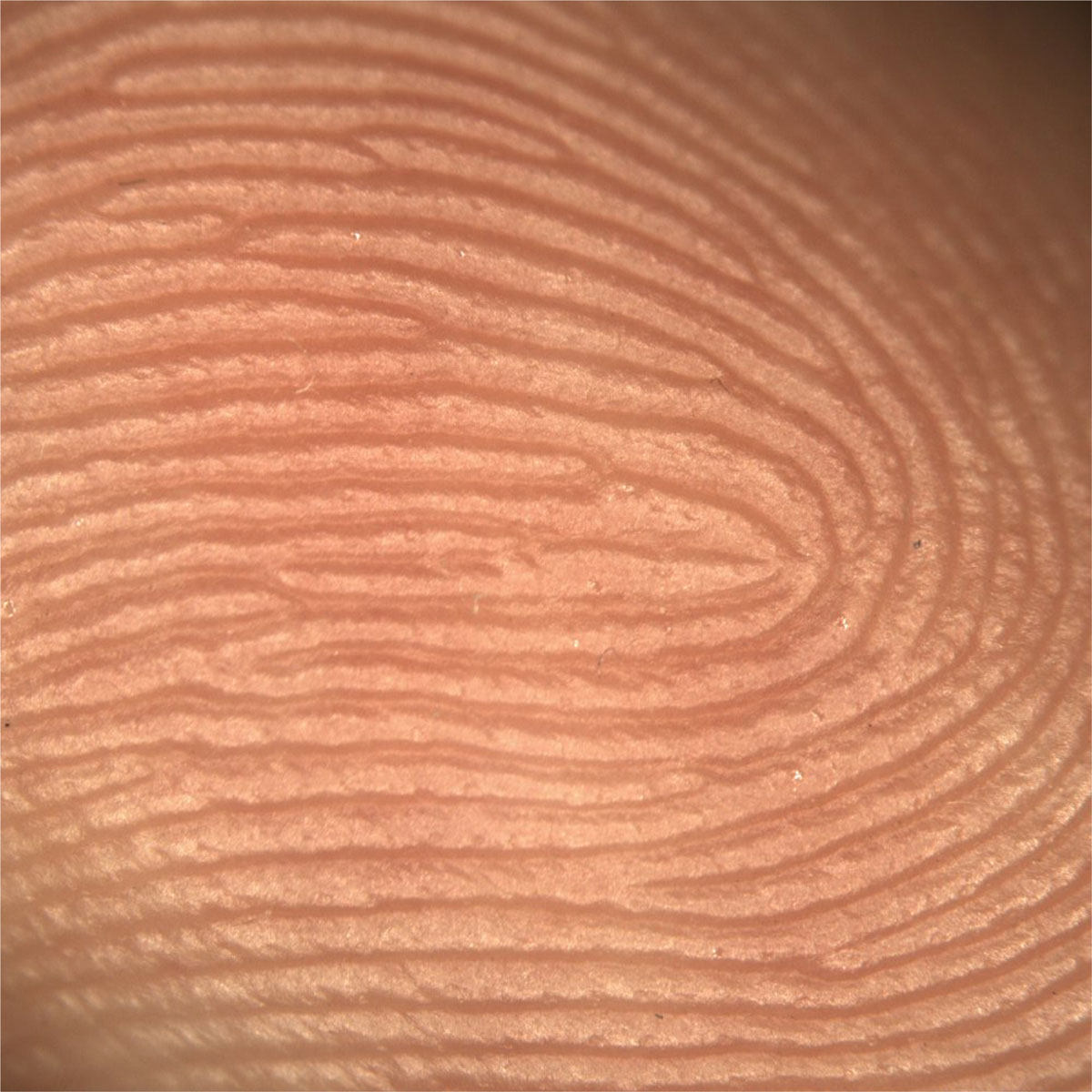
Microscope
In addition, there are other reasons why moles may be different in these locations.
- Sun exposure: The soles of the feet and the palms of the hands are usually less exposed to the sun and therefore may have fewer changes related to sun exposure.
- Pressure and friction: The soles of the feet are subject to increased pressure and friction due to daily activity, which can influence the shape and texture of moles in this area. The palms of the hands are also subject to some friction, but to a lesser extent than the feet. It is believed that this is one of the reasons why melanoma appears on the soles of the feet.Quote
- Genetic differences: Genetics plays an important role in mole formation, and individuals may inherit predispositions to develop certain types of moles on different areas of the body.
Are moles on hands and feet really more dangerous?
Actually, moles on the soles of the feet and the palms of the hands They are NOT more dangerous than moles on the body. This is a concept left over from the older generation of specialists, who did not have adequate diagnostic tools to detect melanoma early and therefore preferred to remove all moles in these locations.
Fortunately, however, things have changed radically over the last few years and we now have a revolutionary tool: the Dermatoscope!
How do we study moles on hands and feet?
Since we introduced the dermatoscope into our routine clinical practice, we are able to make very accurate diagnoses even in areas that were very difficult to evaluate in the past, such as the acral skin.
What is a dermatoscope?

A dermatoscope is a tool that allows dermatologists to examine moles to detect structures that may indicate skin cancer. The polarized light in the dermatoscope eliminates reflections from the skin surface, allowing a clearer view of skin structures and pigmentation patterns, facilitating the identification of malignant skin lesions.
The scientific study that changed everything
In 2004, this study appeared in the prestigious journal JAMA dermatology. Quotewhere dermoscopic criteria for benign pigmented lesions on the hands and feet were defined. Thanks to these criteria, we are now able to differentiate much more precisely the difference between melanomas and moles in acral locations.
It is interesting to note that this article was written by my current bosses, and great friends, at the Hospital Clínic de Barcelona, who are recognized as leading experts in the field of dermoscopy worldwide. Personally, I have a deep respect and appreciation for them because of their significant contribution to this field of dermatology.
What do moles and melanoma on the skin of hands and feet look like?
To better illustrate these images I will show you below some images of what this type of mole looks like in this characteristic location. It is also important to have some clues to know if this mole has benign or malignant characteristics.
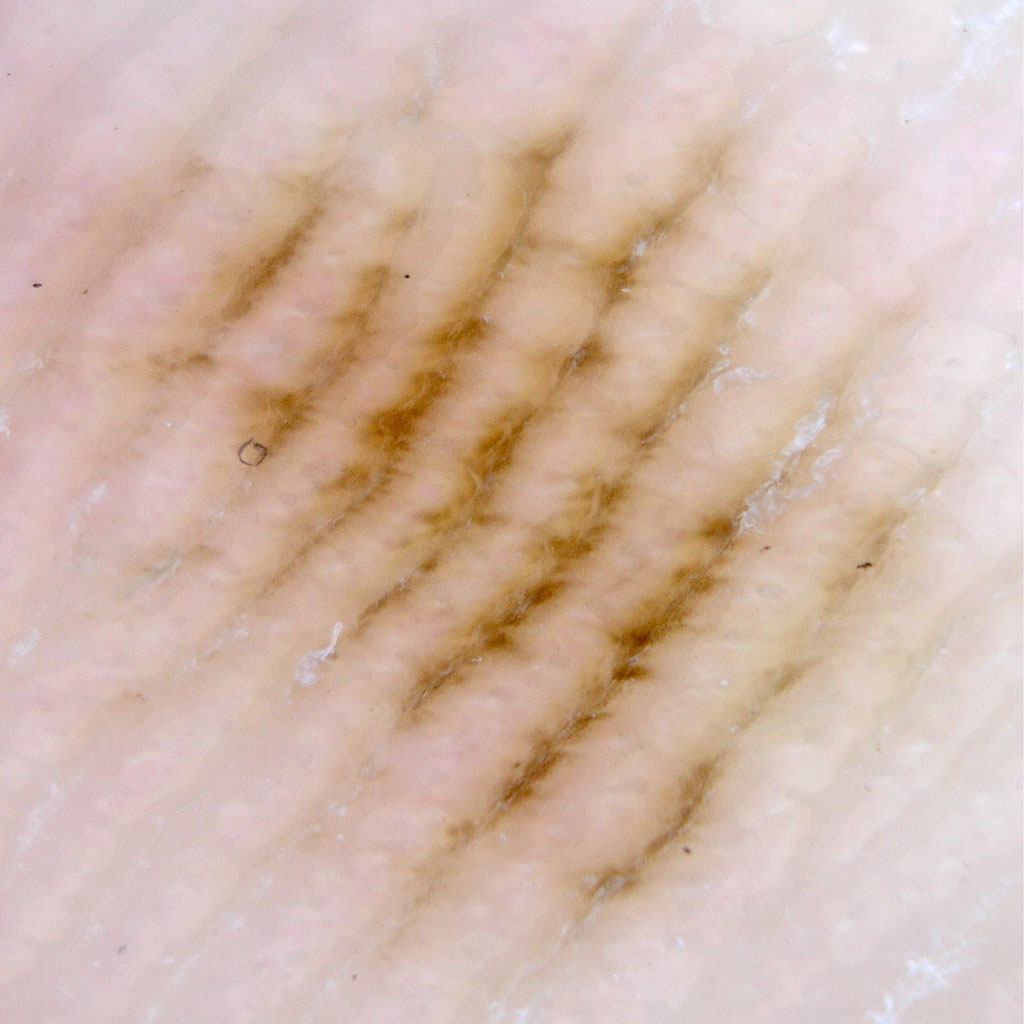
What do moles on the soles of the feet and palms of the hands look like?
Moles on the soles of the feet tend to appear during childhood and adolescence. They can also appear later in life, however it is less common. It is important to know that Moles are stable lesions that will not change or grow over time.and that should reassure us.
Here are some pictures of moles on the soles of the feet and palms of the hands.
Clinical imaging

Dermatoscopic image
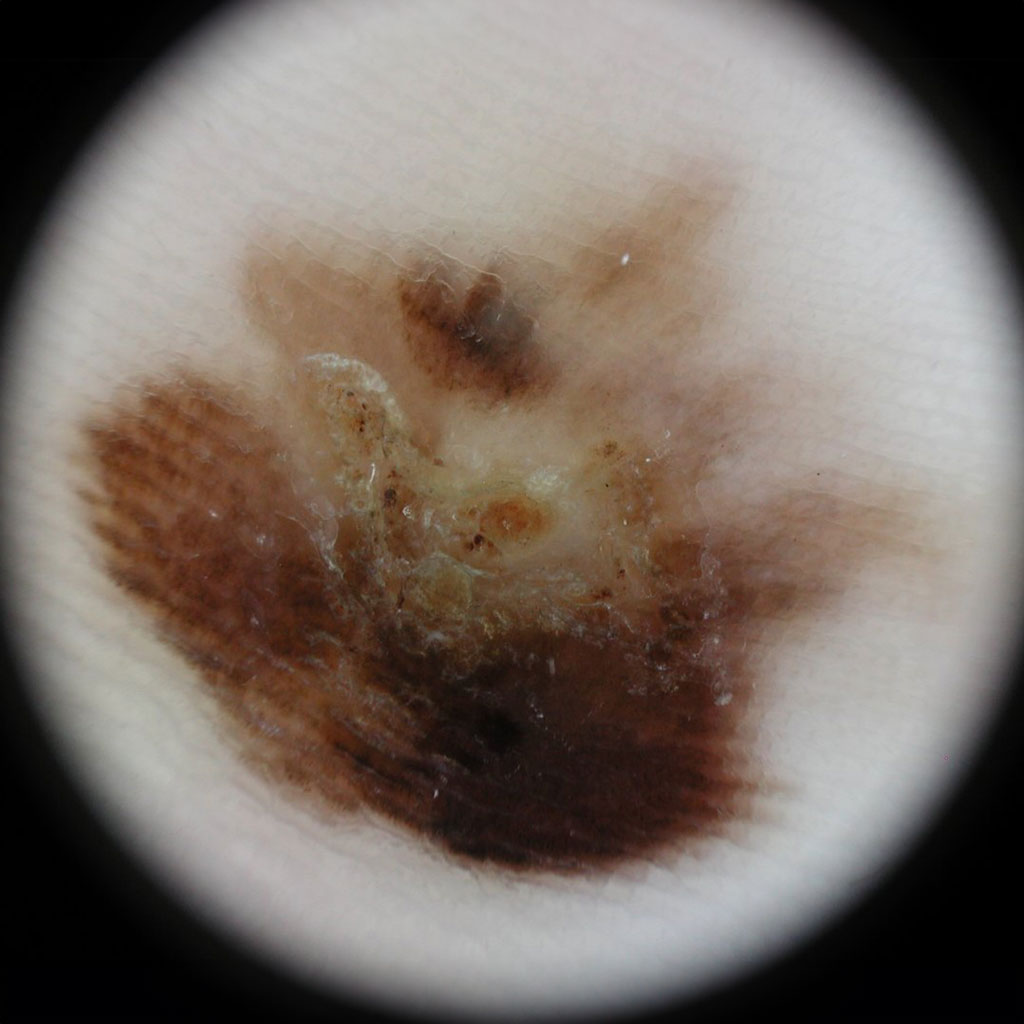
What do melanomas on the soles of the feet and palms of the hands look like?
Melanoma, the most serious type of skin cancer, usually develops in areas of the skin that have been exposed to excessive sunlight, however, It can also do it in places where the sun rarely reaches, like your feet! This type of melanoma is called acral lentiginous melanoma.
The big problem with this skin cancer is that the majority of people with people do not usually check their feet for signs of melanoma, And that's a problem because this cancer sometimes spreads before you know it.
When melanoma develops on the acral skin, it can manifest as a changing mole or spotbut you can also do it in the following ways:
- A pink or red spot or wart that is growing
- A new stain on the site of an injury you had some time ago
- A nonhealing foot ulcer (or an ulcer that heals and comes back)
Melanoma on the foot can sometimes be painful, bleed or itchy, but this is not always the case. In fact, most of the time it can be totally asymptomatic and only manifest itself as a spot that grows.
Here are some images with some examples of this type of melanoma:
Clinical imaging

Dermatoscopic image
Are there people who are more predisposed to develop acral melanoma?
Melanoma is a rare form of skin cancer, accounting for 2% to 3% of all melanoma cases. However, it is the most common type of malignant melanoma in people who traditionally have dark skin, especially in African-Americans and people of Asian and Middle Eastern origin.
And are polka dots on the nails different?
Another very curious place where moles can also appear on the hands and feet, are the nails. In this case, they are different and look like lines of pigment that grow along the nail. I recently wrote a very complete article about moles and melanoma on the nails that you can review here..

Conclusions
The moles on the soles of the feet and palms of the hands are NOT more dangerous than on the rest of the body.. However, this area is more difficult to evaluate because we do not normally look at the soles of our feet. In addition, there is a diagnostic delay in the case of melanoma, because these are areas that are not normally examined or that doctors do not usually check during consultations.
In summary, awareness and vigilance are critical in the early identification of melanoma on the feet and hands. Any suspicious skin changes in this area should be evaluated by a dermatologist to ensure timely diagnosis and treatment.

Do you have doubts about this type of moles?
La entrada Lunares en la planta de los pies y palmas de las manos se publicó primero en Dr. Sebastian Podlipnik.
How to remove warts by a dermatologist?
Before going in depth on how to remove warts, it is crucial to clarify something important. Here in Spain and in Spanish-speaking countries, we usually call "warts" anything with relief on the skin.. Therefore, in this article you will not only learn how to remove warts, but also understand what these "warts" really are and the importance they have on our skin.
That's why I think it's so important to write this article, because we will not only see how to remove warts but we will also demystify a lot of thingssuch as:
- What is really a wart and what is not?
- Which warts are contagious and which are not?
- Can we use home remedies to remove warts?
My name is Sebastian Podlipnik and I am a dermatologist at the Hospital Clínic de Barcelona and in the Dermatological Diagnosis Clinic.

What will I talk about in this article?
What are warts?
In this blog, I want to highlight a crucial point: not all bumps on the skin are "warts". There are various skin growths and excrescences that can have varied diagnoses and should not be confused with warts. It is essential to understand the difference and seek an appropriate diagnosis for each specific case.
Let's see the differences between the two!
1- Viral warts or simply "warts".
The True warts are benign growths on the skin caused by the human papillomavirus (HPV).. As they are produced by a virus, they are the true contagious warts, but they can only be is spread by skin-to-skin contact or by touching contaminated objects. Thus, warts are not transmitted through blood.
There are several types of warts depending on the type of papillomavirus (serotype). we have contracted. In other words, there is not only one type of papillomavirus, but many different types.
The most common are:
- Common or vulgar warts which typically appear on the hands.
- Plantar warts: on the soles of the feet typically in children, although they are also frequent in adults.
- Flat warts which are smaller and smoother and occur mainly on the face of children.
- Genital warts or condylomas which are transmitted by sexual contact and affect the genital and anal area. Depending on the serotype, they could be a risk factor for the development of cervical or penile cancer.

2- Remaining skin bumps and growths
The rest of the "warts" are actually bumps on the skin that come in all shapes and sizes, and there are a lot of possibilities of what they can be. To make it more interesting, the diagnoses will be very different depending on the area of the body that is affected.
Some of the most common are:
- Moles or nevi
- Epidermal cysts
- Sebaceous hyperplasia
- Lipomas
- Seborrheic keratoses
- Angiomas
- Or even skin cancer can present itself as a "wart"!
Each has its own characteristics and requires different treatments. So, if you see any strange bumps or if something changes on your skin, it is very important that you go to a dermatologist. to have it checked. We will give you an accurate diagnosis and tell you what to do in each case.
To make it easier, we will review the main body sites where patients go for "wart removal" and look at the actual diagnoses with representative photos of each diagnosis.
How to remove warts on the eyelids?
In the eyelids we can observe different types of protuberances with different diagnoses. Let's review the most frequent causes for which patients come to my office to eliminate them.
Let's get to it!
Millimetrial cysts of the eyelids

Millium cysts are small yellowish-white bumps that form on the skin. due to the accumulation of keratin. If you have them, see the following link
Eyelid fibromas

Eyelid fibroids are small, benign lumps caused by a overgrowth of connective tissue and fat.
I usually remove them with procedures such as cauterization or CO2 laser, since excellent results are obtained.
Syringomas on the eyelids

Syringomas are small benign protuberances that are related to the sweat glands.
They do not represent a health risk, but can be aesthetically bothersome. Treatment with CO2 laser is an effective and safe option to eliminate syringomas.Quote
How to remove warts on the neck?
95% of the times a patient comes in to have "warts" removed on the neck they are actually acrochordons or fibroids. They are soft growths that protrude from the surface of the skin. Their appearance may vary, but they are usually the size of a grain of rice, and may be flesh-colored or darker.

Facts about acrochordons in the neck
- 95% of neck warts are actually acrochordons or fibroids.
- They are not contagious!
- They are not produced by necklaces or chains!
- Its main cause is genetic!
Cause of acrochordons in the neck
The exact causes of why acrochordons appear on the neck are not fully known, but it is known that they are more likely to be caused by to appear with lon age and on areas of the skin that rub against each other. They are also more common during pregnancy due to hormones, and tend to have a genetic component, i.e., if your parents had them, you are likely to develop them too.
And it is very important for you to know thate are not contagious nor are they caused by the use of neck chains.
Treatment of acrochordons on the neck
Skin tags are usually harmless and there is no medical need to remove them. However, some people choose to remove them for cosmetic reasons or because they are bothersome.
The safest way to remove skin tags is with the help of a dermatologist. My favorite methods due to their speed and excellent results include:
- Cutting with scissors after anesthesia with an anesthetic cream
- CO2 laser
How to remove warts from the face?
In other areas of the face, excluding the eyelids, the reasons for consultation to remove "warts" vary slightly. Here, the The most common lesions are dermal moles, seborrheic keratoses and sebaceous hyperplasias.
Dermal or warty nevi
Dermal or warty nevi are one of the most frequent reasons for consultation I have in the office when it comes to "warts on the face". The nevus or moles arise from the growth of melanocyteswhich are the pigment-producing cells in the skin.
Looking at the graph above, you will see that there are roughly 2 types of moles:
- Nevi or flat moles: are pigmented skin spots found at the level of the epidermis and are usually light or dark brown in color.
- Verrucous or dermal nevi: are raised bumps of pigment in the skin that develop in a deeper layer called the dermis and can be of different colors and shapes.
Here is a before and after of a patient who came in to remove a dermal mole in the pre-auricular region. Look at the result!

Click on the button below and see that I have written a longer article, with a full and detailed explanation of safe and effective methods of mole removal, including options such as surgical and laser removal, as well as tips for aftercare of the treated area.
Seborrheic keratoses

Fortunately Seborrheic keratoses respond very well when properly treated. I leave you a "Before and after" to know the result obtained after CO2 laser treatment of this type of lesions.
In the following link find out all about seborrheic keratoses in my full article! You will find detailed information and useful tips to understand and treat these benign and common skin lesions.
Sebaceous hyperplasia

Sebaceous hyperplasia treated with the CO2 laser looks great! This laser does a precise job of removing those bumps without damaging the surrounding skin. The best part is that the skin recovers quickly and looks much better and smoother after treatment.
Subsequently, I always recommend my patients to use a retinol cream to prevent their reappearance in the future.
How to remove warts from the body?
I also have many patients who come to the office to remove "warts" from the body. In this case some diagnoses are repeated with those we have seen previously, but I will also include other frequent reasons for consultation of my patients.
So we can see quite often:
- Dermal nevus or verrucous moles (see in dermal or verrucous nevi on the face)
- Seborrheic keratoses
- Red moles or angiomas or ruby spots
Seborrheic keratoses on the body
As in the face there can also be seborrheic keratoses on the body. Their frequency increases with age and they probably have a very important genetic component as I mentioned previously.
Often, patients come to the office with these lesions that have been present for years, which are of great aesthetic concern and have affected their self-esteem. Often, they are unaware that it is possible to remove them, but with the right treatment, we can help them to remove them completely.
If you want to know in detail how we eliminate seborrheic keratoses, I recommend you to click on the following link to see the complete process.
Angiomas or red spots or ruby spots

Find out how to remove ruby spots or angiomas in my full article below! Click on the link to see the detailed process and you will also find videos that will show you how we remove them with the laser.
How to remove warts from the armpits?
Almost always patients who come in for underarm wart removal have fibroids or acrochordons. Underarm fibroids are small, benign, soft bumps that can be bothersome because of their location and friction with clothing. You can see more in the section on how to remove warts on the neck that I already talked about this topic.
Removal is a safe and simple procedure that can be performed by methods such as surgical excision, cauterization, cryotherapy or laser, always with prior evaluation by a dermatologist.
A few words about warts and skin cancer
It is important to note that in some cases, warts or bumps on the skin can be a manifestation of skin cancer. While most warts are benign and do not pose a health risk, it is essential to pay attention to any changes in their size, shape, color or texture.
Therefore, before any treatment or wart removal, it is essential to visit a dermatologist for an evaluation to rule out any possible complications.
If you are interested, in this article I leave you a summary of what skin cancer can look like.
Conclusions on how to remove warts
In this article on how to remove warts by a dermatologist, you have learned fundamental things and we have reviewed different diagnoses. It is crucial to differentiate viral warts (HPV) from other skin growths and to avoid self-medication. or home methods that could worsen the situation.
It is key that you leave this issue in the hands of experts for proper treatment. Do not risk with home remedies, better consult a pro to get rid of those warts without drama and with excellent aesthetic results!
In summary, my article gives you the most important fact: trust a dermatologist to say goodbye to warts simply and without drama. Expert hands are the key!
La entrada ¿Cómo quitar verrugas por un dermatólogo? se publicó primero en Dr. Sebastian Podlipnik.
Moles and melanoma on the nail, how to identify them?
Some time ago, I gave a talk at a congress to my dermatologist colleagues about moles and melanoma on the nails. I thought it would be important to share this information with my patients and blog readers. During the talk, I shared several clinical cases of patients who had spots on their nails that turned out to be melanomas. Seeing the interest and concern in the eyes of my colleagues, I realized the importance of spreading this knowledge and raising awareness about the importance of taking care of our nails.
My name is Sebastian Podlipnik and I'm a skin cancer specialist at the Hospital Clinic de Barcelona. During my years of experience I have seen many cases of moles and melanoma on the nail and it is one of the reasons why I decided to write this blog.
In this entry, We will learn how moles look on the nails, how to detect suspicious changes of skin cancer and when to consult a dermatologist.. In addition, I will share with you many pictures of nails so that we can identify them with good images.
I accompany you on this journey of dermatological knowledge!

What will I talk about in this article?
What do moles and melanoma on the nail look like?
Moles are common on our skin and are usually harmless. However, when it comes to moles on the nails, it is important to pay special attention to them.
Often, the following can be observed nail stains brown or black that adopt a linear shape, technically called ".longitudinal melanonychia". They are usually seen as brown or black lines that affect the length of the nail.
Depending on their characteristics they may correspond to benign lesions or even in some cases to malignant lesions such as melanoma. In general terms Moles are small, well-defined lines, while the Melanomas are more chaotic, with larger spots and the pigment may extend beyond the nail.
Lunar
Melanoma
These small brown marks may seem insignificant, but in some cases they could be signs of melanoma, an aggressive form of skin cancer.
Why do moles and melanoma look like brown or black lines?
This is because the cells that produce the pigment (melanocytes) are located in the nail matrix, which as you can see in the following image, is the most proximal area of the nail. If there is an increase of melanocytes (proliferation), either by a mole or a melanoma, the pigment will adhere to the nail plate (nail) and will advance as the nail grows.
What do moles look like on the nails?
Generally speaking, nail moles are very stable lesions and should not change significantly over time. They usually present with a band of pigment that affects only one nail.

Clinical photo of a mole on the nail. Image obtained from European Journal of Pediatric Dermatology.

Dermoscopic photo showing a regular pigmented band corresponding to a nail mole.
What signs should lead one to suspect melanoma of the nail?
There are several signs that may lead us to suspect a malignant lesion of the nail and we will review them so that you have the diagnostic clues. Possibly one of the most important is that a malignant lesion usually only affects 1 nail. If, on the other hand, you notice the appearance of these spots simultaneously on several nails, possibly the cause of the pigmentation is something else that we will see later in the blog.
| That there be progressive changes
You will find that moles and benign nail lesions are very stable, so we do not expect them to grow or change over time. One of the first signs that we will see in melanoma of the nails are progressive changes such as those shown in the following image.
| Triangular shape of the pigment line
Maybe this is a little bit more difficult to explain and understand, but if you remember what I explained previously that melanocytes are located in the nail matrix and then attach to the nail as it grows.
Therefore, if we have a fast growing lesion it will rapidly increase in size in the proximal part of the nail, however the pigment found in the more distal part will be the pigment that "stuck" several months ago to the nail.

Image obtained from Clinics in Dermatology
| Other important signs
There are other important signs to be mentioned that are already present in more advanced lesions. These are:
- Thickness more than ⅓ of the nail: If the band of pigment on the nail measures more than one third of the total width of the nail we should be concerned.
- Pigmentation beyond the nail: If we observe that the brown pigmentation extends to the skin adjacent to the nail.
- Hutchinson's sign: If the pigmentation also affects the proximal nail fold.

Now we are going to see a picture of a patient presenting some signs of malignancy in a nail affected by melanoma. If you have any of these signs, it is important to consult a dermatologist.

Are there other causes of brown and black lines on the nails?
Before I continue, I would like to give you some peace of mind as the appearance of brown or black spots on the nail can have different causesThe most of them are not serious. We have already reviewed moles and melanoma which correspond to a growth of melanocytes (melanocytic proliferation). But, there are also other times when melanocytes can be activated and also produce brown or black lines on the nails.
Classification of nail stains

Generally speaking, we can classify nail stains as longitudinal melanonychia due to melanocyte activation or melanocyte proliferation.
The causes of melanocyte activation can be very broad, and most often several nails are affected at the same time, unlike moles or melanoma that usually affects only one.
The most frequent causes of melanocytic activation are
- Pregnancy
- Trauma
- Nail biting
- Nail infection
- Lichen planus
- Psoriasis
- Viral warts
- Addison's disease
- Hyperthyroidism
- Photosensitivity
- Lupus
- HIV
- Phototherapy
- X-ray exposure
- Antimalarial drugs
- Chemotherapy drugs

Image obtained from bmj case reports
What do we do in the dermatological office when we see a melanonychia?
To properly evaluate a patient with a melanonychia, we perform a series of procedures to establish a diagnosis.
1- physical examination
To begin with, I will conduct an examination complete physic of all your nails, both fingernails and toenails. This involves evaluating any deformities, the presence of melanonychia on multiple nails, as well as the color, shape and size of the affected areas. In addition, I will review your medical history to identify any underlying conditions that may be causing your nail staining.
2- Dermatoscopy (onychoscopy)
The next step in the diagnostic process involves a dermatoscopic examination. I will use a specific type of microscope to closely examine the suspicious areas. During this examination, my main focus will be to determine if there are signs that the melanonychia may be malignant.
3- Take a course of action with the injury
After completing the above two steps, we will assess whether the lesion is benign, suspicious or malignant.
- Benign lesion: If it is very clear to us that the reason for the pigmentation in the nail is benign, we can indicate a treatment to improve or discharge if it does not require further studies.
- Suspicious lesion, but not clearly malignant: Sometimes we will not have enough information to be able to establish a clinical diagnosis of the spot on the nail. In these cases it will be necessary to perform a digital follow-up of the nail or we may also request a biopsy.
- Lesion clearly suspicious of malignancy: In this case, we will directly assess the possibility of nail surgery to remove the lesion completely and biopsy it in its entirety.
Conclusions on moles and melanoma of the nail
When it comes to evaluating nail stains, I recommend that you do it in person. This way, he will be able to examine your spot with dermoscopy and provide you with an accurate diagnosis.

Consultation with an expert
If you have a nail stain of this type that concerns you, it is important that you consult a specialist.
La entrada Lunares y melanoma en la uña. ¿Cómo identificarlos? se publicó primero en Dr. Sebastian Podlipnik.
The best Dermatologist in Barcelona How to choose one?
Choosing the best dermatologist in Barcelona can seem like a challenging and overwhelming task, especially when you are faced with numerous options and advertisements on Google. It is understandable that, in the midst of this avalanche of information, you may feel distrustful and doubtful about who is the right dermatologist to solve your skin problems.
But don't worry! In this blog, I want to share with you the most important aspects that I consider as a dermatologist so that you can make an informed and reliable decision. From my professional perspective, I will guide you through the key elements to consider when choosing the specialist that perfectly fits your needs.

What will I talk about in this article?
Sound education and training
When you have to trust someone to take care of your skin, there is nothing more important than ensuring the dermatologist's training. Education and academic achievement are the first point to consider when choosing the best dermatologist in Barcelona.
Look for professionals who:
- Have a specialization in dermatology recognized by accredited institutions
- Participation in continuing education programs
- Attendance and lectures at conferences and congresses
- Make a contribution to the medical research
Tips
- Check the doctor's Linkedin profile to see his training and specialization.
- Check his professional social networks to assess whether he attends medical congresses and conferences.
Check the specialty of the dermatologist you will visit in the registry of registered physicians in Barcelona.
Although it may seem crazy it is crucial to verify the credentials of the dermatology specialist.Unfortunately, there is a problem of labor intrusion in Spain and many people without the specialty pose as dermatologists.
For this reason, the The Barcelona Medical Association has made available the page of the registry of registered physicians of Barcelona where you can check the doctor's specialty. It is very easy to check:
Step 1: Find your doctor

Step 2: review your specialty

Reputation by peers
I will tell you one of the most important secrets for me: other doctors know who is really good!
So, if you have the opportunity, ask about the reputation of a dermatologist among our professional peers. Our dermatology colleagues are often familiar with our work, professional ethics and level of experience. By obtaining references and opinions from other medical professionals, you can get a more solid idea of the quality of care we can provide.

Have a specialist in the problem you are suffering from
Today the trend in medicine is to sub-specialize, and you'll find that dermatologists do too. At by choosing a dermatologist who specializes in your specific problem, you can be confident that you are receiving expert, personalized care. you need to effectively address your dermatological problems.
Tips
- Check the doctor's website and see what his sub-specialty is.
- Check out their social networks
Updated knowledge
Ensuring that the dermatologist has up-to-date knowledge is critical. Medicine and dermatology are constantly evolving, with new treatments, technologies and approaches emerging on a regular basis.
It is crucial to stay abreast of the most recent advances in our field and participate in continuing education programs. This ensures that we are using the most current and effective techniques and therapies to address your dermatologic needs.
Tips
- Check out the research profiles of this doctor
- See the researcher profile at researchgate.com
- See the publications he has made in pubmed.com
Excellent communication skills
Effective and empathic communication is essential to establish a good doctor-patient relationship. A A good dermatologist will excel in listening attentively to patients, explaining diagnoses and treatments in an understandable manner, and responding to patients' questions and concerns in a clear and respectful manner.
For this point you can also look at the doctor's social networks or his YouTube channel and see if you like how he explains the problems.
State-of-the-art technologies
Dermatology is in constant evolution, and The use of state-of-the-art equipment and technology can make a difference in diagnosis and treatment results. Look for a dermatologist who keeps up with the latest innovations and invests in cutting-edge technology to offer you the best in skin care.
From advanced lasers and devices to non-invasive techniques incorporating artificial intelligence, the use of cutting-edge technologies can improve the accuracy, efficacy and comfort of dermatological treatments.
Sensitivity and empathy
This is possibly one of the most important points as a medical professional. Putting yourself in the patient's shoes and understanding that dermatologic diseases can have a significant emotional impact on patients is critical. Being able to show empathy and sensitivity to patients' concerns and emotions is an essential quality in providing comprehensive care.
Tips
You can indirectly look at the comments that the dermatologist has on Google My Business and see what patients have to say.
Multidisciplinary collaboration with other specialists
Dermatology is interrelated with other medical specialties and collaborating with other medical specialists when necessary is very important to provide comprehensive care to patients. This includes working as a team with other healthcare professionals to ensure the best possible outcome. Therefore, if a specialist also works in a reference hospital in Barcelona, he/she may be in contact with many specialists in other specialties.
Reputation and references
Reputation and referrals are a reflection of the quality of care a dermatologist provides. The best dermatologist in Barcelona will be noted for having a solid reputation and receiving positive referrals from satisfied patients. This demonstrates their ability to deliver successful results and a high level of patient satisfaction.
Tips
To assess this point, you can always look at the dermatologist's comments in Google My Business (more reliable than other platforms as negative comments are not filtered out).
In conclusion, how to choose the best dermatologist in Barcelona?
Choosing the best dermatologist in Barcelona requires time, research and consideration. It is important to look for a professional with a solid educational background, verifiable credentials and up-to-date knowledge.
Also, don't forget to consult the references and opinions of other medical professionalsas well as the experiences of previous patients. Remember that trust and comfort with your dermatologist are critical to establishing a long-term quality care relationship. Your skin is a valuable organ and deserves the best possible care.
In case of doubt, call the dermatologist's office and ask if the dermatologist has experience in treating the specific areas of concern.
Do you think I missed a point? Feel free to comment below.
La entrada El mejor Dermatólogo en Barcelona ¿Cómo elegirlo? se publicó primero en Dr. Sebastian Podlipnik.
How to treat a sunburn?
Sunburn is a reality that affects many people around the world, especially in summer. These burns can be very painful and have serious long-term health consequences.The sunburn may also increase the risk of developing skin cancer. That is why it is important to know how to treat a sunburn properly to avoid complications.
In this blog you will I will show you some treatments and tips for treating sunburn effectively. We will learn together why these burns occur, how to identify them and how to treat them to ensure a quick recovery and avoid adverse consequences.

Types of sunburn
Sunburns are classified into three types: mild burns, moderate burns and severe burns.
- Minor burns are those that cause redness and pain on the skin, but do not cause blistering or scarring.
- Moderate burns are those that cause redness, pain, blistering, swelling and peeling of the skin.
- Severe burns are those that cause scarring of the skin.
Get started as soon as possible!
Skin can burn if it gets too much sun without proper protection from sunscreen and clothing. To help heal and relieve itchy skin, it is important to start treating a sunburn as soon as you notice it.. The first thing to do is to get out of the sun, preferably indoors.
How to treat a sunburn?
Once you are indoors and out of the sun, dermatologists recommend that you follow the following tips to help you learn how to treat a sunburn :Quote
- Take frequent cold baths or showers to relieve pain. As soon as you get out of the bath or shower, gently pat yourself dry, but leave some water on your skin. Next, apply a moisturizer to help retain water in the skin. This can help relieve dryness and tightness of the skin.
- Use a moisturizer containing aloe vera or soy to help soothe sunburned skin. If a particular area is particularly bothersome, you can apply a hydrocortisone corticosteroid cream that you can buy without a prescription.
- Do not treat sunburn with local anesthetic products. "-caine" (such as benzocaine), as they may irritate the skin or cause an allergic reaction.
- Consider taking aspirin, acetaminophen or ibuprofen to help reduce swelling, redness and discomfort.
- Drink more water. Sunburn draws fluid to the surface of the skin and away from the rest of the body. Drinking more water when you are sunburned helps prevent dehydration.
- If you get blisters on your skin, let them heal. Blistering means you have a second-degree sunburn. You should not pop the blisters, as they form to help the skin heal and protect you from infection.
- Take extreme precautions to protect sunburned skin while it heals. Wear clothing that covers your child's skin when outdoors.
Consequences of sunburn
Although it may appear to be a temporary condition, sunburn - the result of excessive exposure of the skin to the sun's ultraviolet (UV) rays - can be a temporary condition. can cause lasting damage to the skin. This damage increases the risk of getting skin cancer and cause premature aging of the skin, so it is essential to protect the skin from exposure to UV rays.
La entrada ¿Cómo tratar una quemadura solar? se publicó primero en Dr. Sebastian Podlipnik.
Page processed in 0.687 seconds.
Powered by SimplePie 1.3.1, Build 20121030175403. Run the SimplePie Compatibility Test. SimplePie is © 2004–2025, Ryan Parman and Geoffrey Sneddon, and licensed under the BSD License.